18100006002 CASE PRESENTATIONS
LONG CASE:
A 70 years old female patient residing in Nalgonda, is a homemaker, presented to OPD with
complaints of- loss of appetite since one week,
- generalised weakness since one week
- fever since 5 days
-burning micturation since 5days
History of present illness-
patient was apparently asymptomatic one week back then she gradually developed loss of appetite since one week which was not associated with nausea, vomiting, associated with generalised weakness
fever since 5 days which was high grade associated with chills and rigors, no diurnal variation, relived on taking medication, not associated with headache, cold , cough
she also started experiencing burning micturation since 5 days associated with low backache , no history of dark coloured urine or blood in urine
no h/o cold, cough, chest pain, palpitations, shortness of breath, pedal edema , reduction in urine output, diarrhoea, constipation, vomiting, nausea, pain abdomen
Past history:
she has been having similar episodes since 2016
she had 1st episode in 2016 it started with fever which was high grade associated with chills and rigors, associated with loss of appetite which were followed by loss of consciousness. she was immideatly rusged to a local hospital where the attenders were told that she had high blood pressure and had high blood sugars. she was diagnosed with UTI and was treated with parenteral antibiotics for 5 days and was discharged on oral antibiotics which she took for one week. since then she had been having recurrent episodes of UTI 2-3times every year. after the 2nd or 3rd episode she started having urinary incontinence for which she consulted a urologist and was said to have weakness of pelvic floor muscles and was advisced pelvic floor muscle strengthning exercises.
28 years back she underwent hystrectomy
25 years back she had complaints of generalised weakness
↓
went to a diagnostic center and got few investigations done
↓
consulted a physician and was diagnosed with type 2 diabetes mellitus and was started on OHAs
↓
she did not take OHAs regularly
during that time she was residing in Saudi Arabia and her husband took her to regular check ups almost every weekend during that period he sugars were under control with OHAs
↓
in 2007 they moved back to India in 2010 she had uncontrolled blood sugars for which she was started on insulin , she started using insulin pen
↓
in 2013 she consulted an endocrinologist and was started on injections Humalog (insulin Lispro) 28 units in the morning and Basalog ( insulin Glargine) 20 units at night
↓
started having tremors, weakness ,excessive sweating , and excessive hunger ( had recurrent hypoglycemic attacks) during which he son Dental surgeon adviced her to reducethe dose of Insulin lispro to 20 units
↓
reviewed with the same endocrinologist and was advisced to stop Insulin glargine and was told to take insulin lispro in the evening also
↓
had recurrent episodes of UTI and got hospitalised for the same
↓
10 years back she had chest pain for which she was taken to a cardiologist and was diagnosed with angina and was started on antiplatelets, statins and isisorbide dinitrate ( SOS) , tab febuxostat 40mg ( for joint pains), vitamin D3 supplementation, and was also advisced tab nitrofurantoin for 20 days since then she was on a regular follow up with the cardiologist every 3 months
she also started having complaints of tingling and numbness in her lower lower limbs and was diagnosed with peripheral neuropathy secondary to diabetes mellitus and was startedon tab. neuroprime plus ( alpha lipoic acid, thiamine, mecobalamine, elemental chromium)
was also diagnosed with CKD and anemia
↓
Diagnosed with Hypothyroidism 5 years back and was started on tab. levothyroxine 50 mcg daily before breakfast
↓
blood sugars were not undercontrol in 2020 consulted an endocrinologist was started on sitagliptin 50mg and metformin 1000mg everyday morning before breakfast along with insulin
↓
in 2020 she was treated at home by her son for the similar episodes
↓
in 2021 march she had complaints of fever , cough and was diagnosed with COVID 19 infection and was hospitalized
there she was treated with Injection remedesivir for 5 days along with parenteral steroids and was later discharged on oral prednisolone and was gradually tapered over 10 days and then stopped
↓
in july she again had another episode of UTI and was again hospitalized
↓
was brought to our center
Personal history: married with 8 children - 4 sons and 4 daughters all are well at present,
no addictions - non smoker non alcoholic
sedentary habit
adequate sleep
no bowel abnormalities
family history- not significant
treatment history:
used insulin lispro (50%) + insulin lispro protamine 25 units in the morning and evening subcutaneously
used - Tab Ecospirin AV 75/10 mg H/S
tab Met -XL initially 25 mg for few years then 5o mg once daily
tab. feburic acid 40mg
tab tenegliptin 20mg then changed to tab sitaglipten 50mg + metformin 1000mg once daily
vitamin D3supplementation
used multiple antibiotics for recurrent UTI- nitrofurantoin, clarithromycin, piptaz, meropenem, levofloxacin
tab isosorbide dinitrate SOS
PROVISIONAL DIAGNOSIS:
A 70 years old lady with Recurrent complicated UTIs with peripheral neuropathy, secondary to diabetes mellitus (type 2) with hypertension with hypothyroidism known case of ischaemic heart disease.
GENERAL EXAMINATION:
patient is conscious, coherent, cooperative and oriented to time, place and person
patient is lying comfortably in supine position
patient is obese and well nourished
Height- 151 cms
Weight - 57 kgs
BMI - 25.0 kg/m2
face- wrinkled
eye- no abnormalities, baggy lower eyelids, pallor present, no xanthelasma or xanthomas
no cyanosis
oral cavity- lost all teeth, mucosa appears normal
nails- normal, no clubbing
no thyroid enlargement
no lymphadenopathy
neck veins- not distended
skin- normal, No pigmentation ,No scars, No atrophic changes
pulse- 110 beats per minute in supine position in right radial artery, regular rhythm, high volume, vessel is thickened, all other peripheral pulses are felt and are normal
BP: 110/80 mmHg in Right arm in supine position
100/80 mmHg in standing position
Respiration-- 20 breaths per min, thoraco-abdominal type
temperature- normal at the time of examination
feet-no pedal edema, no ulcers or calluses
GENITOURINARY SYSTEM EXAMINATION:
perabdomen- no abnormalities, no visible scars and sinuses
foleys catheter is insitu and is connected to urobag
no renal lump felt
renal angle- no tenderness
urinary bladder- empty
local examination - pubic hair-sparse distribution
labia majora, minora- atrophied
external uretheral meatus- no discharge, healthy
per vaginal examination bimanual examination
bilateral fornices free , non tender
anterior fossa normal
posterior fossa normal
Vault intact - no palpable masses felt, no tenderness
NERVOUS SYSTEM EXAMINATION
patient is conscious, cooperative, alert and oriented to time place and person
cranium and spine -normal, no abnormalities
speech- normal
Recent and remote memory intact
1. CRANIAL NERVES
CRANIAL NERVE | TEST | RIGHT | LEFT |
I | Sense of smell i) Coffee ii) Asafoetida |
+ + |
+ + |
II | i) Visual acuity – Snellens Chart ii) Field of vision – Confrontation test iii) Colour vision – Ishihara chart iv) Fundus | 6/6 Normal Normal Normal | 6/6 Normal Normal Normal |
III, IV, VI | i) Extra-ocular movements ii) Pupil – Size iii) Direct Light Reflex iv) Consensual Light Reflex v) Accommodation Reflex vi) Ptosis vii) Nystagmus viii) Horners syndrome | full 4mm Present Present Present Absent Absent No | full 4mm Present Present Present Absent Absent No |
V | i) Sensory -over face and buccal mucosa ii) Motor – masseter, temporalis, pterygoids iii) Reflex a. Corneal Reflex b. Conjunctival Reflex c. Jaw jerk | Normal Normal
Present Present Present | Normal Normal
Present Present Present |
VII | i) Motor – nasolabial fold hyeracusis occipitofrontalis orbicularis oculi orbicularis oris buccinator platysma ii) Sensory – Taste of anterior 2/3rds of tongue(salt/sweet) Sensation over tragus iii) Reflex – Corneal Conjunctival iv) Secretomotor – Moistness of the eyes/tongue and buccal mucosa |
Present Absent Good Good Good Good Good
Normal
Normal
Present Present
Normal |
Present Absent Good Good Good Good Good
Normal
Normal
Present Present
Normal |
VIII | i) Rinnes Test ii) Webers Test
iii) Nystagmus | Positive Not lateralised
Absent | Positive
Absent |
IX, X | i) Uvula, Palatal arches, and movements
ii) Gag reflex iii) Palatal reflex | Centrally placed and symmetrical
Present present |
|
X1 | i) trapezius ii) sternocleidomastoid | Good Good | Good Good |
XII | i) Tone ii) Wasting iii) Fibrillation iv) Tongue Protrusion to the midline and either side | Normal No No Normal | Normal No No Normal |
Right. Left
Bulk: inspection UL normal normal
LL normal normal
palpation. UL Normal normal
LL normal normal
LL: 5/5 5/5
LL lost in distal parts on both sides
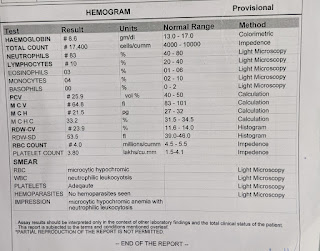
Investigations
FINAL DIAGNOSIS:
- Recurrent complicated urinary tract infections
- Complicated Fungal UTI
- Asymmetric Peripheral neuropathy secondary to Diabetes mellitus type 2
- Diabetic nephropathy
- known case of Ischaemic heart disease, Hypertension, Hypothyroidism
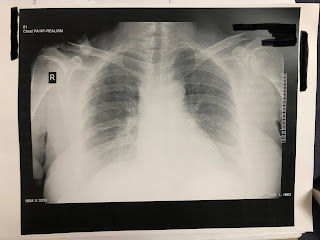
A 43 old male patient resident of nalgonda ,farmer by occupation ,presented to casualty with complaints of :
Low grade Fever since 1 year .
Cough with sputum since 1 year
Complaints of neck pain since 6 months
Weakness of all both lower limbs since 6 months .
HOPI :
Patient was married at age of 25 and have 3 children , one son and two daughters . He is farmer by occupation . He is occasional alcoholic and chronic smoker (1-2 packs/day) since 20 years . He was apparently alright till 33 years of age , then in view of generalised weakness pt went for routine evaluation and got diagnosed with diabetes mellites- type 2 and is using OHA since 10 years . He takes his medication regularly .
Patient had history of fever since 1 year which was low grade not associated with chills and rigors, intermittent, associated with diurnal variation and night sweats.
He also complains of cough with scanty white color ,mucoid expectorant since 1 year, non foul smelling, non blood tinged . No diurnal variation of cough and no chest pain .
He went to local rmp and got symptomatic treatment .
He later developed neck pain , which was sudden in onset gradually progressive . No history of trauma .No radiation .
He then developed weakness of both lower limbs which was insidious in onset ,gradually progressive in nature over 6 months . He had difficulty in standing and walking .No history of upper limb weakness .
Past history:
No h/o similar complaints in past.
K/C/O DM-2 since 10 years on Glimi -m1 tablet .
Not a known case of HTN/EPILEPSY/CVA/CAD/TB
Personal history:
Mixed diet with normal appetite and normal bowel/bladder movements
H/o alcohol consumotion since 90ml weekly twice since 20 years.
H/o smoking (1-2 pacs per day ) since 20 years .
General Examination:
He is a thin built man, who was conscious, coherent
PR of 80bpm ,regular rhythm ,normovolemic .
Bp - 110/80mmhg
Temp - 98.3 F
SpO2 - 99%
RR - 22 cpm
GRBS - 120 mg/dl.
Head to toe examination:
Hair - Black, thick, non easily pluckable. No lesions over the scalp.
Eyes - No pallor, no icterus.
General head & neck examination - No abnormalities. No lymphadenopathy.
Axial- Tenderness over cervical spine +
Fingers & Nails - Clubbing +
Lower limbs - No pedal edema .
1. CRANIAL NERVES
CRANIAL NERVE | TEST | RIGHT | LEFT |
I | Sense of smell i) Coffee ii) Asafoetida |
+ + |
+ + |
II | i) Visual acuity – Snellens Chart ii) Field of vision – Confrontation test iii) Colour vision – Ishihara chart iv) Fundus | 6/6 Normal Normal Normal | 6/6 Normal Normal Normal |
III, IV, VI | i) Extra-ocular movements ii) Pupil – Size iii) Direct Light Reflex iv) Consensual Light Reflex v) Accommodation Reflex vi) Ptosis vii) Nystagmus viii) Horners syndrome | full 4mm Present Present Present Absent Absent No | full 4mm Present Present Present Absent Absent No |
V | i) Sensory -over face and buccal mucosa ii) Motor – masseter, temporalis, pterygoids iii) Reflex a. Corneal Reflex b. Conjunctival Reflex c. Jaw jerk | Normal Normal
Present Present Present | Normal Normal
Present Present Present |
VII | i) Motor – nasolabial fold hyeracusis occipitofrontalis orbicularis oculi orbicularis oris buccinator platysma ii) Sensory – Taste of anterior 2/3rds of tongue(salt/sweet) Sensation over tragus iii) Reflex – Corneal Conjunctival iv) Secretomotor – Moistness of the eyes/tongue and buccal mucosa |
Present Absent Good Good Good Good Good
Normal
Normal
Present Present
Normal |
Present Absent Good Good Good Good Good
Normal
Normal
Present Present
Normal |
VIII | i) Rinnes Test ii) Webers Test
iii) Nystagmus | Positive Not lateralised
Absent | Positive
Absent |
IX, X | i) Uvula, Palatal arches, and movements
ii) Gag reflex iii) Palatal reflex | Centrally placed and symmetrical
Present Present |
Present Present |
X1 | i) trapezius ii) sternocleidomastoid | Good Good | Good Good |
XII | i) Tone ii) Wasting iii) Fibrillation iv) Tongue Protrusion to the midline and either side | Normal No No Normal | Normal No No Normal |
-------------------------------------------------------------------------------------------------
SHORT CASE- 2:
35 year old man working as a food caterer presented to our OPD with the chief complains of
Dyspnea at rest since 5 days
Cough with expectoration since 5 days
Bilateral pedal edema since 4 days
Abdominal distension since 3 days
He was a regular alcoholic since the past 10 years and an occasional smoker. He apparently was completely alright until one morning in November 2019 when he had high fever with chills and visited a local hospital where he got admitted, he says the fever was intermittent and more at nights and was often followed by sweating and was diagnosed with malaria for which he received treatment.
In Dec 2019, the following month, he says he started feeling breathless while climbing up the stairs which progressed over the next 5 days to such an extent that he even felt dyspneic even at rest and had dry cough on and off. He says that his dyspnea and cough aggravated on laying in bed. He gradually developed bilateral pedal edema followed by abdominal distension over the next few days which alarmed him and he decided to pay a visit to a doctor. He visited a local hospital and was put on some medications ( no documentation ) which patient couldn't recall of. Since it did not improve his symptoms he visited our hospital in January 2020.
He however gave no complaints of palpitations, nausea, vomiting, profuse sweating.
He also gave no complaints of reduced urine output, hematuria, forthy urine.
No complaints of burning micturation, diarrhea, vomiting, pain abdomen.
PAST HISTORY:
Since the past 10 years he has been consuming around 180 ml of whiskey everyday. He also tells that he would occasionally smoke cigarette once in a while along with his friends. In those 10 years he never paid a visit to his hometown due to financial issues and decided not to get married anytime soon as he wanted to settle the financial issues his family was facing.
Not a known case of Diabetes, Hypertension, Also no history of CAD, CVA, Bronchial Asthma, Pulmonary Koch's.
On presentation to our hospital:
He was obese with central obesity
His pulse rate was 100 bpm
Blood pressure - 110/70mmhg
RR - 21 cpm
Spo2 - 98% on Room Air
Temp - 98.6 %
GRBS - 151 mg/dl
GENERAL EXAMINATION:
He weighed 98 kgs and his abdominal girth measured 100 cm
He had no pallor, icterus, clubbing, cyanosis, lymphadenopathy
He had bilateral pitting type of pedal edema present upto his knees
JVP was raised
SYSTEMIC EXAMINATION:
CARDIOVASCULAR:
Inspection:
Shape of the chest - Ellipsoid
No dilated veins, scars, sinuses
No cutaneous lesions
No breast abnormalities
Palpation:
Apex beat palpated in 6th ICS 1 cm lateral to MCL
No palpable pulsations in aortic or pulmonary area or tricuspid area
No palpable pulsation
No palpable epigastric pulsations
No palpable pulsations in sternoclavicular area
Auscultation:
Muffled S1,S2 +
RESPIRATORY SYSTEM EXAMINATION:
Inspiratory crepitations in Bilateral in IAA, ISA
PER ABDOMEN:
soft
Non tender
No organomegaly
Bowel sounds +
CENTRAL NERVOUS SYSTEM EXAMINATION:
Normal
PROVISIONAL DIAGNOSIS:
HEART FAILURE SECONDARY TO
? VIRAL MYOCARDITIS
? ALCOHOLIC
REPORTS:
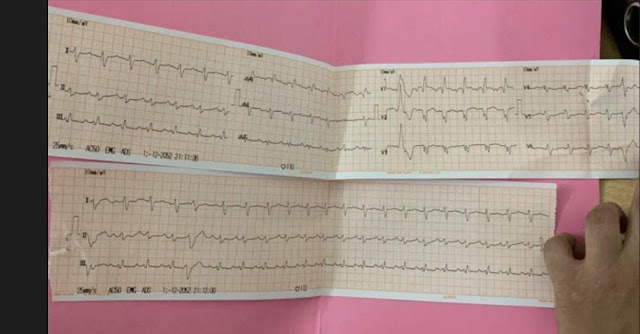
ECG:
His blood picture, renal and liver parameters were in within the normal range.
On routine investigations his HbA1c was found to be 8.4 %.
His Ultrasonography of abdomen revealed Grade 1 fatty liver ( probably secondary to his alcohol intake), mild ascites, Right moderate pleural effusion.
2DEcho was done which revealed that all the 4 chambers to be dilated with an ejection fraction of 27, global hypokinesia, severe MR, trivial AR, severe LV dysfunction with mild PAH, dilated IVC (2.3cm)
A diagnosis of HEART FAILURE WITH REDUCED EJECTION FRACTION - 27%
DENOVO DETECTED TYPE 2 DIABETES MELLITUS
TREAMENT ADVISED:
he was started on
1. Tab Lasix 80mg in the morning, 40mg in the afternoon and evening
2. Tab Isosorbide mononitrate 10mg twice a day
3. Tab Hydralazine 25mg
4. Tab Telma 40mg
5.Tab Metformin 500mg once a day
and was advised for fluid of less than 1 litre and salt restriction of less than 2grams/day
He was advised for a coronary angiogram for which he visited Hyderabad. CAG was performed on 24th of January 2020 which turned out to be normal and he was started on Tab Vymada 50mg and Tab Met XL 12.5mg
( Sacubitril 26 mg and Valsartan 24 mg) along with Tab Ecosprin AV (75/20)
On regular at home monitoring of blood glucose levels which were within the normal range, he stopped taking Tab Metformin.
On 14th March 2020 he paid a visit to our hospital with the similar complains and a review scan of 2DEcho was done which revealed end point septal separation distance to be increased and Tab Vymada was increased to 100mg.
On July 28th, 2020 he presented to our OPD with the complains of Dyspnea at rest since 5 days which apparently aggravates when the patient is in supine posture and he also complains of occasional cough with scanty mucoid, non blood tinged sputum especially while he is asleep. He says he developed bilateral pedal edema extending upto his knee over the past 4 days followed by abdominal distension.
Patient appears to have gained weight with abdominal girth measuring 116cm and he weighed 101 kg
He weighs 93 kgs now
He appeared to be in respiratory distress with a respiratory rate of 28 cycles per minute and his saturation was at 98 % on room air.
His heart was beating at 120 bpm with a blood pressure of 100/70mmhg.
He was afebrile.
He had Icterus
His JVP was raised
CVS:
On palpation:His apex beat was in 6th intercostal space, 1cm lateral to midclavicular line.
On auscultation, S1 S2 +
His lungs were clear on auscultation
His abdomen was soft to palpate and bowel sounds were heard.
CNS: Normal
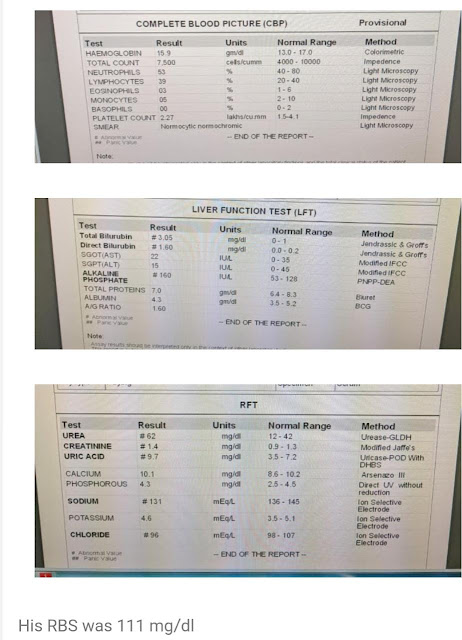
Hemogram:
Hb - 13 g/dl
TLC - 7000 cells/cumm
Platelet count - 2.28 L/cumm
Complete Urine Examination:
showed no albumin, sugars, RBCs
2-4 Pus & epithelial cells
Renal Function Test :
Urea - 53 mg/dl
Creatinine - 1.4 mg/dl
Uric Acid - 9 mg/dl
Calcium - 9.6 mg/dl
Phosphorus - 3.3 mg/dl
Sodium - 133 mEq/L
Potassium - 4 mEq/L
Chloride - 98 mEq/L
Liver Function Test:
Total Bilirubin - 4.60 mg/dl
Direct Bilirubin - 2.42 mg/dl
AST - 56 IU/L
ALT - 44 IU/L
ALP - 129 IU/L
Total Proteins - 6.2 gm/dl
Albumin - 3.9 gm/dl
His 2Decho showed dilated chambers with global hypokinesia, ejection fraction of 26 %, severe MR, mild TR, Trivial AR, mild pericardial effusion, mild PAH and IVC measuring 1.7 cms.
The Patient is currently on fluid and salt restriction
Along with INJ LASIX 40MG TID
TAB VYMADA 100 MG BD
TAB VALSARTAN 80MG OD
TAB MET XL 12.5MG OD
TAB DYTOR PLUS 10/25 OD

























Comments
Post a Comment