Fever since 3 months
Cough with expectoration since 2 months
Dyspnea on exertion since 2 months
Vomiting since 2 months
Decreased appetite and weight loss over last 2 months
Dark coloured stools since 2 weeks.
History of presenting illness:-
Patient was apparently asymptomatic 3months back till when he attended his relative function where he consumed alcohol for 2days ( Around 8 beers) following which after 2days he developed high grade fever though not associated with chills & rigors or Night sweats and it subsided with medication for 1 week but from then he's having on & off fever.
The following month he started experiencing productive cough with mucoid expectoration, blood tinged amounting to 2 to 3 cup's per day it's foul smelling . Cough is more in sitting position & slightly relieved by Lying down on bed & It's more during day time than in night.
He also started feeling difficulty in breathing on walking for small distances . It's progressive & currently he has to take a break After walking for 100meters of distance.
He's having 2 to 3 episodes of vomiting daily containing food particles.
He also complains of loss of appetite and unintentional weight loss of around 10 kgs over the past 3 months from 72kgs to 62kgs.
History of black colour stools since 2weeks not associated with mucus or foul smelling.
No h/o chest pain, palpitations, syncopal attacks, profuse sweating, Orthopnea or paroxysmal nocturnal dyspnea
No h/o Headache, seizure, weakness of arms or legs
No h/o Regurgitation of food or epigastric burning pain.
Past history:-
Not a k/c/o Hypertension, Diabetes mellitus, Asthma, epilepsy, Tuberculosis or any heart diseases. No past history of allergies or surgeries.
Personal history:-
Diet- mixed
Appetite- decreased
Sleep-adequate
Bowel & bladder- normal
Occasional alcoholic, Occasional smoker.
Family history:-
No h/o similar complaints in family members
Drug history:-
Patient visited around 4 hospitals in past three month's where he's given multiple antibiotic injections, Antipyretics.. Etc
No h/o any drug allergies .
Summary at end of history:-
A 26yr old male who's a construction worker by occupation and who's an occasional smoker presented with persistent fever, cough with blood tinged expectoration and decreased appetite associated with weight loss since 2months and black color stools since past 2weeks and had a history of reccurent hospital visits & intake of medications for these complaints in past 2months with no history of Hypertension, diabetes or any contact with TB.
Differentaial diagnosis:-
Lung consolidation
Lung abscess
General physical examination:-
Patient conscious, coherent, cooperative
Moderately built & moderately nourished.
Height- 165cm
Weight- 55kgs
BMI- 20.2
Temperature - 100.6f
PR - 94bpm, Regular & normal volume, No radioradial or radio femoral delay.
All peripheral pulses felt
BP - 100/70mmhg Right arm supine position
RR - 28cpm, Abdominothoracic type.
Spo2 at 98 % on room air.
Pallor +nt
Icterus -nt
Cyanosis -nt
Clubbing -nt
Lymphadenopathy -nt
Edema -nt
No Nicotine staining over hand's, lips or any visible wasting of hand muscles
Spine appears normal
SYSTEMIC EXAMINATION:-
RESPIRATORY SYSTEM-
Patient examined in sitting position
Inspection:-
Upper respiratory tract - oral cavity, nose & oropharynx appears normal.
Chest appears Bilaterally symmetrical & elliptical in shape
Respiratory movements appear equal on both sides and it's Abdominothoracic type.
Trachea central in position & Nipples are in 4th Intercoastal space
No signs of volume loss
No dilated veins, scars, sinuses, visible pulsations.
Palpation:-
All inspiratory findings confirmed
Trachea central in position
Apical impulse in left 5th ICS, 1cm medial to mid clavicular line
Cricosternal distance is 3finger breadths.
MEASUREMENTS-
chest circumference- 31 inches at expiration & 32 inches at full inspiration
Chest expansion- 2.5cm
Right left
Hemithorax- 15.5 inches 15.5 inches
Hemithorax expansion- 1/2inch 1/2inch
AP diameter- 7 inch
Transverse diameter- 12 inches
AP/T ratio - 0.58
Respiratory movement's:- decreased on Right side.
https://drive.google.com/file/d/1t2cmYVK6yu6o3VcOhsvibeqqIxISZ8uS/view?usp=drivesdk
https://drive.google.com/file/d/1t41C_0FklIuSHq68BDEh0uEK43_srWWy/view?usp=drivesdk
Tactile vocal phremitus- increased in right Infraaxillary & infra scapular area.
Aegophony & whispering pectorloquy present in right Infraaxillary & infra scapular area
Percussion:-
Right left
Supraclavicular- Resonant (R) (R)
Infraclavicular- (R) (R)
Mammary- (R) Dull
Axillary- (R) (R)
Infra axillary- Dull (R)
Suprascapular- (R) (R)
Interscapular- (R) (R)
Infrascapular- Dull (R)
Auscultation:-
Right Left
Supraclavicular- Normal vesicular (NVBS)
Breath sounds (NVBS)
Infraclavicular- (NVBS) (NVBS)
Mammary- (NVBS) (NVBS)
Axillary- (NVBS) (NVBS)
Infra axillary- Tubular B.S (NVBS)
Suprascapular- (NVBS) (NVBS)
Interscapular- (NVBS) (NVBS)
Infrascapular- Tubular B. S (NVBS)
ABDOMEN :-
Inspection :
shape of abdomen appear normal & symmetrical
No Generalised/Localised distension seen.
All quadrants moving equally with respiration
Umblicus is central & inverted
Skin over the Abdomen- Looks normal
No visible Scars/Sinuses/Dilated/Prominent veins / peristalsis/Pulsations .
Palpation :
All Inspectory findings confirmed
Mild Tenderness in right hypochondrium
No Guarding/ Rigidity
Edge of liver is palpable on deep inspiration Spleen is not palpable
Percussion:-
Liver span is 15cm from right 4th ICS to right coastal margin along mid clavicular line
Spleenic dullness noticed in left coastal margin
Auscultation:-
Normal bowel sounds heard, no renal bruit heard.
CARDIOVASCULAR SYSTEM:-
Apical Impulse felt in left 5th ICS, no parasternal heave or precordial bulge felt
S1S2 heard
No murmers heard.
CENTRAL NERVOUS SYSTEM:-
Higher mental functions intact
No FND, pupils-NSRL.
Cranial nerves- Intact
Motor & sensory systems- Normal.
PROVISIONAL DIAGNOSIS:-
Right lung lower lobe consolidation.
INVESTIGATIONS:-
Hemogram-
Hb- 9gm/dl
Tlc- 13,700cells/cu mm
Plt- 4lakh/cu mm
Rft:
urea- 10mg/dl
Creatinine- 0.9mg/dl
Sodium-129mEq/l
Potassium-4.1mEq/l
Chloride-94mEq/l
Lft:Total bilirubin-2.28mg/dl
Direct bilirubin-0.52mg/dl
SGOT- 109 IU/L
SGPT-12IU/L
Alkaline phosphate- 313IU/L
Total proteins - 7.5gm/dl
Albumin-2.7gm/dl
Esr- 90mm
PT-INR - 20 sec & 1.1
APTT- 39sec
BT & CT - 2min & 5min
HIV, HBSAG, HCV- Negative
ECG:-
USG chest:- Consolidatory changes noted in right lower lobe .
Chest xray-
USG abdomen- A large hypoechoeic lesion measuring 8cm × 8cm in right lobe of liver.
Final diagnosis:- Amoebic liver abscess with rupturing into pleural cavity with Right lung basal consolidation.
Initially conservative management is planned
Treatment:-
1.Inj. Metronidazole 750mg/iv/Tid
2.inj.Ceftriaxone 1gm/iv/bd
3.Inj.pantoprazole 40mg/iv/OD
4.inj paracetamol 1gm/Iv/sos
5.Tab.paromomycin 500mg/Tid
6.syp.Ambrolyte 5ml/Tid
7.Temperature/Respiratory rate /blood pressure/SpO2monitoring.
Treatment & vitals charting:-
Discussion:-
Amoebic liver abscesses most commonly noticed in the age group of 20–45 years and have been noted infrequently in the extremes of ages , with an adult male to female ratio of 10:1 . Our case is of a 26-year-old male patient who presented with the complaint of fever,Cough with Expectoration that's blood tinged, SOB, weight loss for the past three months.
The diagnosis of amoebic liver abscess is sometimes difficult since its clinical manifestations are highly variable, like in our patient who presented with a long standing cough with blood tinged expectoration , intermittent high-grade fever, and progressive dyspnoea & weight loss in spite of not having symptoms like right upper quadrant abdominal pain, jaundice, , the patient still had the disease.
We report a case of Right lung lower lobe consolidation with central liquefaction secondary to an Ruptured amoebic liver abscess that was misdiagnosed as pneumonia & he was been on multiple antibiotics in outside hospitals . Pleuro-pulmonary amoebiasis is easily confused with other illnesses, and it is treated as pulmonary TB, bacterial lung abscess, and carcinoma of the lung .
Aspiration and drainage of pus from thoracic empyema usually will be helpful but in our case it's not presented as empyema
Also, it has been recommended that amoebic liver abscess be treated with metronidazole or tinidazole plus a luminal amoebicide (eg. paromomycin or iodoquinol) even if the intestinal infection is not documented .
Imaging techniques such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) have excellent sensitivity for the detection of a liver abscess and were used with our patient, but these techniques cannot distinguish amoebic abscesses from pyogenic abscesses or necrotic tumor. The diagnosis of an amoebic liver abscess is confirmed with either serologic or antigenic testing. It can also be coupled with stool microscopy and antigen testing of the stool, with or without evaluation for the parasite in the hepatic abscess fluid.
Due the combination of findings in the imaging studies like hepatomegaly, pleural effusion with thick loculated collection, obliteration of costophrenic angles, left subdiaphragmatic collection, and involvement of the right lung which suggested an basal consolidation of the right lung, the patient was treated with a percutaneous liver abscess drainage. Following drainage, the fever improved dramatically as he continued to be under observation.
Some literature indicates that percutaneous needle aspiration or catheter drainage may be helpful for large abscesses (over 5-10 cm), in particular, if the diagnosis is uncertain, if there is an initial lack of response, or if a patient is very ill, suggesting impending abscess rupture, while some authors have had higher thresholds of maximum diameter >10.5 cm and intervention only in the absence of response to drugs . Henceforth, for those cases that fail to respond to the conventional management, interventions such as needle aspiration, catheter drainage, or surgical interventions can be employed as required.
Link's to similar case report's
-------------------------------------------------------------------------------------------------
SHORT CASE- 1:
A 44 year old male patient , farmer by occupation came to OPD with chief complaints of
Pedal edema since 3 months
Shortness of breath since 2months
HISTORY OF PRESENT ILLNESS
The patient was apparently asymptomatic 3months back then he developed bilateral pedal edema pitting type, initially it's below ankle & subsided in early morning's , later it's gradually progressed to below the knee and not assocaited with diurnal variation.
He then developed shortness of breath since 2months ,insidious in onset & gradually progressed from grade 1 to grade 2 to 3 currently.
He's also having peri orbital edema & facial puffiness predominantly in morning since 2mnths
He has decreased urine output since 2mnths
No h/o hematuria, fever, chest pain, palpitations, diaphoresis, syncopal attacks
HISTORY OF PAST ILLNESS:-
He has tested positive for covid-19, 3 months
Back & recovered after using medication
known case of Hypertension since 1 year [on tab CILACAR 10mg - morning, 20mg - night].
Not known case of DM ,Asthma, TB,Epilepsy , CAD
PERSONAL HISTORY
He is married
Occupation - farmer
Diet - Mixed
Appetite - Normal
Bowels - Regular
Micturition - decreased urine output
He has no known allergies
Occasional Alcoholic since 20 years and stopped 3 months back.
No smoking
FAMILY HISTORY
No significant family history
DRUG HISTORY
He has been using Tab. CILINDIPINE 10mg - morning, 20mg -night for Hypertension since 1 year.
SUMMARY AT THE END OF HISTORY:-
A 44yr male patient farmer by occupation who's an occasional alcoholic presented with c/o pedal edema, Sob & decreased urine output with a past history of hypertension and Not a k/c/o DM/Asthma/CAD.
Differential diagnosis:-
Chronic kidney disease
GENERAL EXAMINATION
Patient is conscious,coherent, cooperative and examined in well Lightned room.
VITALS
Pulse rate -94bpm
Respiratory rate - 28cpm/min
BP - 140/90mmHg
Temperature - Afebrile
SpO2 - 98% at room air
GRBS - 141mg%
PHYSICAL EXAMINATION
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing of fingers/toes - absent
Lymphadenopathy - absent
Edema of feet- present,pitting type
SYSTEMIC EXAMINATION
CARDIOVASCULAR SYSTEM
Jvp elevated
Apex beat in left 5th ICS 1cm lateral to mid clavicular line
S1 and S2 heard
No thrills/parasternal heave / murmers heard
RESPIRATORY SYSTEM - Vesicular breath sounds heard in all area's
- No wheezing
- No adventitious sounds heard
ABDOMEN:-- No tenderness
- No palpable mass
- No free fluid
- No Audible bruits
- Liver and spleen are not palpable
- Bowels sounds are heard
CNS
- Conscious,normal speech
- No signs of meningeal irritation
- Normal gait
- Cranial nerves are intact
- Motor system normal
- Sensory system normal
- Reflexes normal
DIAGNOSIS:-Chronic kidney disease secondary to hypertension.
INVESTIGATIONS29/7/2021
ULTRASOUND
ECG
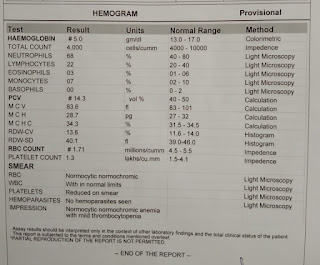
HEMOGRAM
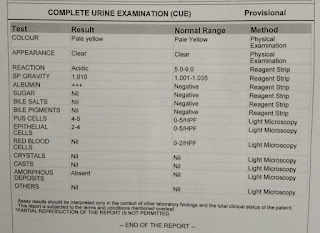
COMPLETE URINE EXAMINATION
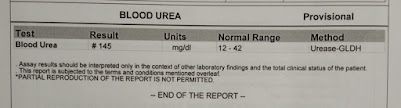
BLOOD UREA
SERUM ALBUMIN
TOTAL SERUM PROTEINS(A/G RATIO)
SERUM CREATININE
4/8/2021SERUM ELECTROLYTES
SERUM IRON
PROVISIONAL DIAGNOSIS
Chronic Renal Failure
TREATMENT
T.Lasix 40 mg PO/BD
T.Cilacar 10 mg PO/OD
T.Nodosis 500mg PO/OD
T.orofer XT PO/BD
T.Cilacar 20 mg PO/OD
Inj.Erythropoietin 4000IU (weekly twice)
Fluid Restriction <1.5L/day
Salt restriction <4gms /day
-------------------------------------------------------------------------------------------------
SHORT CASE- 2:
A 35yr old female patient who's a bank employee by occupation came to casuality with chief complaints of involuntary movement's of right upperlimb & lowerlimb since afternoon 2pm.
History of presenting illness:-
Patient was apparently asymptomatic till today morning, when she developed mild weakness of her right upperlimb & lowerlimb for which she went to local hospital & got few medications & later it subsided, she then attended her bank work where at around 2pm she had sudden involuntary movement's of right upperlimb & right lowerlimb which lasted for 2 to 3 minute's, She had around 5 similar episodes with a time gap of 10minutes.
They're associated with post ictal drowsiness & are not associated involuntary micturition/defaecation/uprolling of eyeballs/ Tongue bite/deviation of mouth/automatic behavior like running, walking about,Violent behavior.. Etc.
She had an similar episode in casuality & she's having post ictal confusion & drowsiness .
From the next day she's drowsy & complained of headache & vomitings.
No h/O palpitations/syncopal attacks/facial deviation/dysphagia/chest pain/ orthopnoea /PND/Neck pain/Projectile vomiting/
Past history:-
No h/O similar complaints in past
Not a k/c/O Hypertension/Diabetes mellitus/ Asthma/epilepsy/TB/CAD/Migraine/Thyroid disorders/psychiatric disorders.
Drug history:-
No known drug allergies/No history of any chronic medications/Oral contraceptive pills intake.
Family history:-
No h/O similar complaints in family members.
Personal history:-
Sleep- Adequate
Appetite- normal
Bowel & bladder - regular
No addictions.
Summary at the end of history:-
A 35yr old female who's a bank employee came with complaints of repeated episode's of involuntary movement's of right upperlimb & right lowerlimb since afternoon which are associated with post ictal confusion & drowsiness & later she had headache & vomitings.
Differential Diagnosis:-
Complex partial seizures secondary to Cerebrovascular accident/ cerebral venous thrombosis.
General examination :-
Pt is drowsy
No pallor/icterus/cyanosis/ clubbing Lymphadenopathy/ edema/
Temperature - Afebrile
Pulse rate -90 beats per minute ,regular, normal volume ,vessel wall normal ,no radio-radial or radio femoral delay, All peripheral pulses felt.
Bp- 110/70mmhg in both arm's supine position
Respiratory rate- 20cpm
Grbs - 109mgdl
SYSTEMIC EXAMINATION:-
Central nervous system-
Patient is drowsy.
GCS - E3V3M3
Pupils- Normal size & reactive to light.
Cranial nerves- corneal reflex +nt
No fixed gaze seen, patient is able to look at all sides on repeated verbal commands.
Vestibulooccular reflex intact.
Motor system:-
BULK- Appears normal on both sides
TONE - Right Left
Upper limb- Normal Normal
Lower limb- Normal Normal
POWER - couldn't be tested. But the patient is moving all her limbs on bed.
Right Left
Reflexes-
Biceps. + +
Triceps. + +
Supinator. + +
Knee. - -
Ankle. - -
Superficial reflexes
Corneal. + +
Conjunctival. + +
Plantars. Extensor. Extensor
Sensory system:-
Moving her body to Deep pain & crude touch in all areas of body.
Anterior Spino thalamic Tract:-
Crude touch: + +
Lateral Spino thalamic Tract:-
Pain. + +
Temperature. Cannot be examined
Posterior column : cannot be examined
Fine touch. -
Vibration. -
Joint position. -
Rombergs. -
Cortical : Cannot be elicited
Two point discrimination -
Tactile localization. -
Stereognosis. -
Graphesthesia. -
Gait : cannot be examined
Sign's of meningeal irritation:-
No neck stiffness .
Brudzinski sign absent
No kernigs sign
Cardiovascular system:-
Apical Impulse felt in left 5th ICS,
No visible pulsations in neck
No parasternal heave or precordial bulge felt
Both heart sounds S1S2 heard
No murmers heard.
Respiratory system:-
Bilateral air entry present
NVBS, No added sounds heard.
Provisional diagnosis:-
Acute complex partial seizures of Tonic clonic variety involving Right upperlimb & Right lowerlimb secondary to CVA/CVT.
Investigations:-
Hemogram-
Hb- 12gm/dl
Tlc- 4,700cells/cu mm
Plt- 3.4lakh/cu mm
Rft:
urea- 10mg/dl
Creatinine- 0.9mg/dl
Sodium-139mEq/l
Potassium-4.1mEq/l
Chloride-99mEq/l
Lft:
Total bilirubin-1.28mg/dl
Direct bilirubin-0.52mg/dl
SGOT- 69 IU/L
SGPT-12IU/L
Alkaline phosphate- 113IU/L
Total proteins - 7.5gm/dl
Albumin-3.7gm/dl
Esr- 18mm
CUE- No pus cells/rbc/proteinuria
Fundoscopy:- Normal.
Loss of flow void in Superior saggital sinus region.
TREATMENT:-
1.Inj Levetericetam 1gm/Iv/Stat followed by
Inj.Levetericetam 500mg/Iv/Bd
2.Inj pantoprazole 40mg/iv/od
3.Inj.mannitol/100ml/Bd
4.Ryles tube insertion & feeding.
5.Temp/pr/Bp/SpO2 monitoring
6.Inform SOS, if seizure reccurs.
Here's the Link to video of her seizures.


























Comments
Post a Comment