18100006010 CASE PRESENTATIONS
LONG CASE:
A 45 year old male, daily wage labourer came to the casuality with
CHIEF COMPLAINTS :
Imbalance while walking since 3 days
associated with Swaying to both the sides since 3 days.
Involuntary movements of the extremities since 3 days.
HISTORY OF PRESENT ILLNESS:
patient was apparently asymptomatic 3 days back then in the morning after he had his
breakfast he noticed
*imbalance while walking along with swaying on both the sides which was sudden in
onset, progressive in nature , associated with generalized weakness and falls without loss of
consciousness.
*involuntary movements of the extremities particularly upper limbs since 3 days,
symmetrical, which was aggravating while trying to reach an object and relieving with
rest,interrupting with his daily activity.
No history of buckling of limbs
No history of stiffness of limbs
No history of difficulty in getting up from squatting position
No history of any difficulty in rolling over the bed.
No history of otorrhea or any hearing loss or any earache.
No history of giddiness or lightheadedness or palpitations, dry skin
No history suggestive of wash basin attack
No history of difficulty in wearing slippers or any slippage of chappals.
No history of any root pain or paresthesias or numbness
No history of neck pain or neck stiffness or blurring of vision or projectile vomitings.
No history of urinary incontinence or retention or diarrhea or constipation.
No history of any speech abnormality or anything suggestive of cranial nerve abnormality.
No history of fever or headache
No history of waxing or wanning of symptoms.
No history of any behavioural changes
No history of weight loss or loss of appetite.
No history of intake of toxins.
No history of joint pains or rash
No history of bulky stools or loose stools.
PAST HISTORY:
Known case of epilepsy and on medication since 8 yrs(Tab PHENYTOIN 100MG/TID)
Not a known case of diabetes or hypertension or thyroid problems or tuberculosis.
No history of any serious illness in the past or any hospital admission
No history of similar complaints in the past.
DRUG HISTORY:
History of excessive intake of phenytoin in the past 20 days for the fear of precipitating seizures.
PERSONAL HISTORY:
Regular diet
Regular bowel and bladder
Disturbed sleep since past 1 month( due to anxiety and depression probably due to loss of
his brother)
Occasionally Alcoholic.
Occasional Smoker : smokes 1 pack (20 cigarretes) in a week ,0.5 pack years
FAMILY HISTORY:
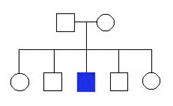
Born on non consanguinous marraige.
achieved appropriate developmental milestones.
No history of similar complaints in the family.
SUMMARY:
GENERAL EXAMINATION:
Patient is conscious ,coherent and cooperative , comfortably lying on bed.
Well built, moderately nourished, BMI of 22kg/m2.
No pallor/ icterus /cyanosis/clubbing/ kylonychia /lymphadenopathy/edema
Hypertrophy of the gums present.
No signs of Neurocutaneous markers or any skin rash
No hyperpigmentation of knuckles.
No signs of nutritional defeciency like chelitis or angula stomatitis or purpura or thinning
of hair or dermatitis or bruising.
No spine abnormalities
No signs of skeletal deformities like pes cavus , short neck.
No detectable KF rings or sunflower cataract or telangiectasias.
VITALS :
PULSE : regular rhythm
82 BPM
good volume
normal charecter
normal vessel wall thickening
no radioradial or radiofemoral delay.
peripheral pulses felt.
BLOOD PRESSURE: right arm supine position.
132/90mm of hg
RESPIRATORY RATE: 22CPM, regular, abdominothoracic type.
TEMPERATURE : afebrile
SYSTEMIC EXAMINATION:
CNS :
Right Handed person, studied upto 10th standard.
HIGHER MENTAL FUNCTIONS:
Conscious, oriented to time place and person.
MMSE 26/30
speech : normal
Behavior : normal
Memory : Intact.
Intelligence : Normal
Lobar Functions : Normal.
No hallucinations or delusions.
CRANIAL NERVE EXAMINATION:
1st : Normal
2nd : visual acuity is normal
visual field is normal
colour vision normal
fundal glow present.
3rd,4th,6th : pupillary reflexes present.
EOM full range of motion present
gaze evoked Nystagmus present.
5th : sensory intact
motor intact
7th : normal
8th : No abnormality noted.
9th,10th : palatal movements present and equal.
11th,12th : normal.
MOTOR EXAMINATION: Right Left
UL LL UL LL
BULK Normal Normal Normal Normal
TONE hypotonia hypotonia hypotonia hypotonia
POWER 5/5 5/5 5/5 5/5
SUPERFICIAL REFLEXES:
CORNEAL present present
CONJUNCTIVAL present present
ABDOMINAL present
PLANTAR withdrawal withdrawal
DEEP TENDON REFLEXES:
BICEPS 2 2 2 2
TRICEPS 2 2 2 2
SUPINATOR 2 2 2 2
KNEE 2 2 2 2
ANKLE 1 1 1 1
SENSORY EXAMINATION:
SPINOTHALAMIC SENSATION:
Crude touch
pain
temperature
DORSAL COLUMN SENSATION:
Fine touch
Vibration
Proprioception
CORTICAL SENSATION:
Two point discrimination
Tactile localisation.
steregnosis
graphasthesia.
CEREBELLAR EXAMINATION:
Finger nose test
Heel knee test
Dysdiadochokinesia
Dysmetria
hypotonia with pendular knee jerk present.
Intention tremor present.
Rebound phenomenon .
Nystagmus
Titubation
Speech
Rhombergs test
SIGNS OF MENINGEAL IRRITATION: absent
GAIT:
wide based with reeling while walking, unsteady with a tendency to fall
unable to perform tandem walking.
CVS EXAMINATION:
S1 S2 Present
No murmurs or added sounds
RESPIRATORY SYSTEM EXAMINATION:
Bilateral airway entry
No added sounds.
PER ABDOMEN EXAMINATION:
Soft and nontender.
No organomegaly present.
FINAL DIAGNOSIS:
FUNCTIONAL : ATAXIA
ANATOMICAL: CEREBELLUM
PATHOLOGICAL:
ETIOLOGICAL: ? DRUG INDUCED(PHENYTOIN)
WORKUP:
CBP:
HB 11.2
TLC 12000
PLATELET 2.02L
ESR 23
LFT Within normal limit
RFT Within normal limit
ECG
CXRAY
A 60 years old female presented to the casualty with complaints of fever associated with chills and abdominal pain.
CHIEF COMPLAINTs
➤Fever for the past 6 days.
➤Pain abdomen for the past 3 days
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 6 days ago after which she developed high grade fever associated with chills, insidious in onset, progressive, not subsiding with medication, continuous type
Pain abdomen , sudden in onset, pricking type, in the epigastrium and right hypochondrium which gets aggravated on right lateral position and relieved with sitting posture, associated with nausea and reduced appetite, no association with intake of fatty food
No complaints of burning micturition.
No complaints of cough, cold or shortness of breath.
No complaints of heartburn or flatulence.
No complaints of heamatemesis or maleana.
No complaints of dysphagia.
No complaints of constipation or diarrhoea.
No history of yellowish discolouration of eyes or high coloured urine.
No history of weight loss
No history of any blood transfusion
No history of any high risk behaviour
HISTORY OF PAST ILLNESS
Not a known case of hypertension, diabetes, bronchial asthma, epilepsy.
k/c/o tuberculosis and took complete treatment.
No history of similar complaints in the past.
DRUG HISTORY
➤No significant drug history or intake of toxins.
PERSONAL HISTORY
➤Occupation: Daily waged labor working in Cotton fields.
➤Patient is married
➤Patient takes mixed diet but has a decreased appetite.
➤Bowel and bladder movement is normal and regular.
➤occasional Alcoholic , non smoker.
- sound sleep
FAMILY HISTORY
➤No significant family history.
MENSTRUAL HISTORY:
G 3 P 4 L 4 A 0
Attained menarche at the age of 20 years, with good flow and volume.
Attained menopause at age of 42 years.
SUMMARY:
60 year old female with high grade fever and abdominal pain confined to
right upper quadrant ,acute in onset, without any alcohol history .
Possibly case of
1) Acute Liver injury (?infective etiology)
2)Acute Cholecystitis.
GENERAL EXAMINATION
Patient is well built, well nourished.
➤Pallor : Not seen
➤Icterus : Not seen
➤Cyanosis : Not seen
➤Clubbing : Not seen
➤Lymphadenopathy : Not seen
➤Edema : Not seen
- No signs of chronic liver cell failure
- No signs of nutritional deficiency.
VITALS
➤Temperature : 101℉
➤PR : 108 beats per minute
➤BP : 100/70 mmHg
➤RR : 24 cycles per minute
➤SpO2 : 95% in room air
➤Blood Sugar (random) : 100mg/dl
SYSTEMIC EXAMINATION
ABDOMINAL EXAMINATION
INSPECTION
➤Shape - Scaphoid, with no distention.
➤Umbilicus - Inverted
➤Equal symmetrical movements in all the quadrants with respiration.
➤No visible pulsation,peristalsis, dilated veins and localized swellings.
PALPATION
➤SUPERICIAL :Local rise of temperature in right hypochondrium with tenderness
and localised guarding and rigidity.
➤ DEEP : Mild enlargement of liver, regular smooth surface , rounded
edges soft in consistency, tender, moving with
respiration non pulsatile
➤No splenomegaly
➤Abdominal girth : 78cms.
➤xiphesternum to umbilicus distance was equal to umbilicus to pubic distance.
PERCUSSION
➤Hepatomegaly : liver span of 16 cms with 4 cms extending
below the costal margin
➤Fluid thrill and shifting dullness absent
➤puddle sign absent
➤Traubes space : resonant
AUSCULTATION
➤ Bowel sounds present.
➤No bruit or venous hum.
NO LOCAL LYMPHADENOPATHY
PER VAGINAL AND PER RECTAL EXAMINATION : NAD
CARDIOVASCULAR SYSTEM EXAMINATION
➤s1 and s2 heard
➤Thrills absent.,
➤No cardiac murmurs
RESPIRATORY SYSTEM
➤Normal vesicular breath sounds heard.
➤Bilateral air entry present
CENTRAL NERVOUS SYSTEM EXAMINATION
➤Conscious and coherent
PROVISIONAL DIAGNOSIS :
ACUTE HEPATITIS (? INFECTIVE)
INVESTIGATIONS :
DAY 1
USG ABDOMEN
 |
USG REPORT IMPRESSION- Multiple liver abscess with largest measuring 5*5 cms in the 7th segment of liver , with 40 to 50% of liquefaction , hepatomegaly with liver span of 18.5 cms. CT SCAN   |
 |
XRAY CHEST-POST TB CHANGES |
A 48 yr old male, farmer by occupation & resident of Nakrekal came to casualty with
LFT
BLOOD UREA